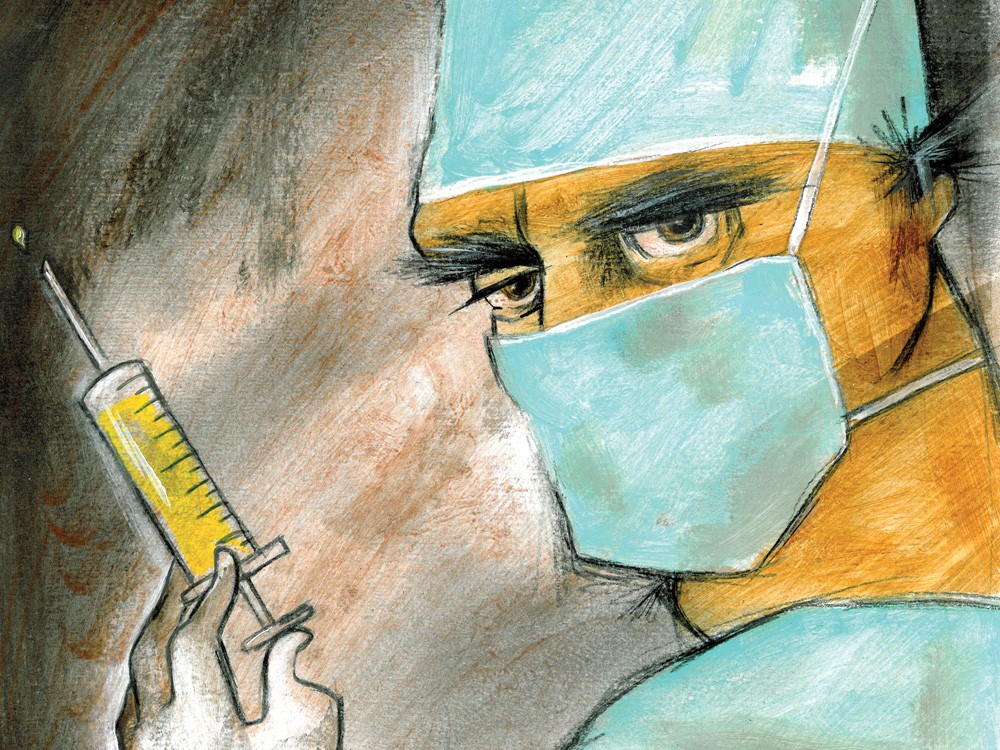
Dr. Mitchell Moffat’s name first appears on page six of the “The Report.” The language around his name is dry and diplomatic: “non-compliance,” “standard of care,” “self-prescribing.”
But then, after the bureaucratic descriptors, two words appear with a startling finality: “License surrendered.”
He was no longer a doctor. Not in Idaho, anyway.
When Moffat’s name appeared on the Idaho State Board of Medicine’s January 2010 report on charges of wrongdoing, it was the end of a long road for him. He was first suspended for two weeks from a Connecticut hospital in 2000 for swearing at a pregnant, Spanish-speaking patient over her inability to speak English.
Then he was arrested in Connecticut in 2007 for writing illegal narcotics prescriptions, and completed a rehabilitation program instead of jail time. Just two years later, he received a license to practice medicine in Idaho and took a job at North Idaho Medical Care in Post Falls. By 2010 he was kicked out of rehabilitation programs in Washington and Idaho and forced to give up his Idaho license.
Even after the string of problems, Moffat was apparently unfazed. He applied for a license to practice in Maine. He wrote in that application that his Idaho license surrender had been “an administrative technicality only.”
The Maine State Board of Licensure denied his application because of his previous behavior. He appealed it.
They denied it — again, once and for all — this February.
Moffat is far from being the only one dinged by state regulatory agencies, but his transgressions may be the most egregious. His name appeared with six others on Idaho’s tally of disciplined doctors. In Washington, the Department of Health sends out its own lists — twice a month.
The Inlander attempted to contact numerous health care professionals in Eastern Washington and North Idaho who were listed in releases from the past year, but they either refused comment or did not return multiple calls.
Struggle To Be Fair
The action against Moffat was one of 5,652 disciplinary orders issued nationwide in 2010 against physicians and physician assistants who are monitored by state medical boards.
They’re all tracked in nationwide databases and their names are released to the public twice a month in Washington and two to three times a year in Idaho.
In the last year, charges ranged from failing to pay licensing fees to theft and drug and alcohol abuse.
Through the releases put out by the state’s regulatory agencies, the charges are blunt and to the point:
- “Michelle Marie Hopwood … was convicted of ... delivery of methamphetamine within 1,000 feet of a school bus stop.”
- “Anthony D. Pfeiffer … massaged a client’s breast and exposed buttock during a massage session. He was convicted of indecent liberties for this conduct in 2010.”
- “Andrew N. Singleton … mistreated a patient by yelling at her, slapping her, and using excessive force.”
“You put your life in the hands of the physician and you just have to hope and trust,” says Mary Leonard, associate director of the Idaho State Board of Medicine.
In a profession built on that hope and trust, the discipline system is complex and riddled with contention. Some say it’s doing its job to protect the public. Others argue it’s focusing too much on providers’ small missteps.
The Process
Mike Farrell, a Washington Department of Health attorney who looks into complaints against physicians and physician assistants, says the process starts when complaints are submitted to the state’s Quality Assurance Commission. The commission only regulates physicians and physician assistants, but other boards made of medical professionals and public members oversee nurses, chiropractors, physical therapists, dentists and others.
After reviewing complaints, the group decides whether each is worthy of investigation and sends the ones that are — about 75 percent, Farrell says — to an investigator.
Investigators look to coworkers and medical records for evidence of malpractice.
“It’s a position that’s really important,” says James Smith, chief investigator for the department. “We are the front line of public protection.”
An attorney and an individual commissioner review and investigate each complaint before it’s sent back to the whole group, which meets eight times a year to review investigations and decide on discipline.
The commission decides whether to dismiss the case or issue some charge of malpractice. All charges are approved by the attorney general’s office and mailed to the doctor.
The notices are not convictions, but they are public information, hence the regular newsletters. Throughout investigation and charges, unless there’s an “imminent danger to public health,” the doctor is free to practice, Farrell says.
Next follows an extensive process where the physician can admit wrongdoing or deny the allegations and appeal the case. Eventually, they’ll either be deemed innocent or face consequences from fines to license suspension.
When medical professionals have had their licenses revoked in another state, no matter the reason, Washington is unwilling to grant them new licenses.
Idaho is more forgiving. Instead of just denying applicants with questionable histories, the Idaho State Board of Medicine demands a lengthy interview and documentation of any past discipline, addictions and participation in rehabilitation programs.
Those with histories of abusing patients or providing poor care are unlikely to receive Idaho licenses, Leonard says. Those who’ve struggled with substance abuse will probably get a second chance. The unique perspective of doctors monitoring doctors means there’s an understanding of the nature of substance abuse, Leonard says. “Drug addiction is considered to be like a disease, so if it can be successfully treated and the person will enroll in rehabilitation, then we’re glad to work with them and give them a second chance,” Leonard says.
The Idaho board trusts rehabilitation programs like those Mitchell Moffat went through in Idaho and Washington, Leonard says, but imposes additional requirements on licensees who’ve had problems. They have to attend regular Alcoholics Anonymous or Narcotics Anonymous meetings, submit to random urine screenings, see a board-approved psychiatrist and find a coworker to monitor them and submit quarterly reports about their behavior. And they have to share that baggage with their next employer.
Some medical offices, especially those in rural areas with fewer doctors, are willing to accept physicians under these stipulations, Leonard says, but many aren’t.
Tough Justice?
After a series of events she blames on misunderstandings, nursing assistant Clare L. Marshall, 46, was fired from her job at a Spokane Valley nursing home and put on an 18-month probation by the Washington commission in 2010. She was accused of making inappropriate comments to one patient and inappropriately touching another; Marshall maintains both incidents were accidental, but she says she had no witnesses to back up her claims of innocence.
Before her probation was over, Marshall was able to find a new job at another retirement home in town.
She and some others in the field say Washington’s discipline process has become bogged down with small concerns. Not everyone being disciplined sold drugs or hurt their patients, they say, so not everyone deserves harsh punishment.
“There’s been so much true abuse in the past in nursing homes that they’ve gone to extremes of going overboard,” she says. “I understand they have to protect patients, but I think it’s just a shame what happened to me.”
If health-care professionals reject the claims made against them, they can first appeal to their medical board or commission, then to the courts. In Idaho, the details of allegations against a provider are confidential during the appeal process, but are made public afterward. In Washington, the first chance for health professionals to appeal is once the commission has issued an order of some type of disciplinary action. Then, the allegations and order are public, and so is the appeal, which is directed to superior court.
Jeffry Finer, an attorney at Spokane’s Center for Justice who has gone through the appeals process with a client, says the system can cast a guilty shadow because names are released even while allegations are being appealed.
“The process where those records become public is muddied when the records are based on convictions that are not final,” he says.
Finer also faults the commission’s priorities. Recent embarrassments have created political pressure, he says, and made the group too quick to judge and too focused on minor issues.
“In an effort to avoid the past failures and to properly monitor, they’ve ramped up the rules in such a way that folks can get caught up in this in good faith and get chewed up and spit out,” he says. “The result is to not only call out the bad apples but anyone who looks like they might have a soft spot.”
Leonard, from Idaho’s medical board, says Washington isn’t alone in facing those criticisms. She’s heard Idaho doctors complain that they’re being punished for something plenty of their colleagues are doing without getting caught. Or that once an investigator starts looking into their practice over one complaint, they could end up being punished for other things, like sloppy record keeping or over-prescribing.
“Those physicians that are disciplined probably always feel like they shouldn’t be,” Leonard says.
No Wiggle Room
But the disciplinary systems states do have, and their perceived shortcomings, aren’t up for discussion, says Farrell, the Washington health department attorney. They’re matters of law.
“We have to keep in mind that the medical commission is a creature of statute,” he says. “It does require statements of charges to be made public. It doesn’t mean they’re guilty of anything. Those are just allegations.”
Leonard stresses that because medicine is a profession where patients put the utmost trust in the people taking care of them, boards and commissions have to be dedicated. There might always be Mitchell Moffats, she says, because there may never be enough people or money in state medical boards to keep the closest eye on every doctor.
So she thinks patients have to be just as dedicated as board members. Patients should ask their doctors questions, she says: Where did you go to medical school? Are you board-certified? Have you done this procedure before? And they shouldn’t hesitate to file a complaint if they’re worried.
“Sometimes after just a complaint, we’ve heard from physicians that it made them step back and re-evaluate how they were giving care and how they were treating patients as people,” she says.